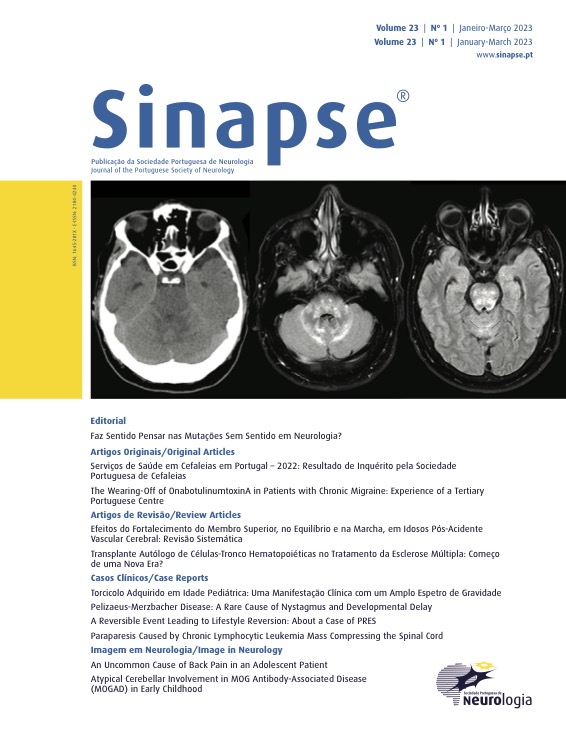
Doença de Pelizaeus-Merzbacher: Uma Causa Rara de Nistagmo e Atraso do Desenvolvimento
DOI:
https://doi.org/10.46531/sinapse/CC/230012/2023Palavras-chave:
Doença de Pelizaeus- Merzbacher/diagnóstico, LactenteResumo
Pelizaeus-Merzbacher disease (PMD) is an X-linked leukodystrophy of the central nervous system characterized by a developmental arrest in myelin formation. It is classified into five phenotypes, with different severity. The most common clinical features are nystagmus, spasticity, tremor, ataxia, and hypotonia. A 11-month-old child was referred to the Neuropediatric Unit due to nystagmus, hypotonia, and developmental delay. Brain magnetic resonance imaging showed signs of diffuse hypomyelination (absence of the T2 low signal in the supratentorial white matter). Molecular analysis revealed a duplication in the PLP1 gene, confirming the diagnosis of PMD. PMD should be considered in infants with nystagmus, hypotonia, and cognitive impairment. Neuroimaging supports the diagnosis, and it should be confirmed by genetic testing. Since no definitive treatment is available, management of this disorder is mainly symptomatic and a multidisciplinary approach for these patients is essential for an improvement in their quality of life.Downloads
Referências
Waldman AT. Pelizaeus-Merzbacher disease. UpToDate. [accessed Jan 2022] Available at: https:// www.uptodate.com/contents/pelizaeus-merzbacherdisease?search=pelizaeus%20merzbacher&source=search_ result&selectedTitle=1~7&usage_type=default&display_ rank=1. Access on august 2020.
Javadikooshesh S, Zaimkohan H, Pourghorban P, Bahramim F, Ebadi N. Pelizaeus-Merzbacher-Like Disease 1 Caused by a Novel Mutation in GJC2 Gene: A Case Report. Iran J Med Sci. 2021;46:493-97. doi: 10.30476/IJMS.2021.87126.1736.
Koeppen AH, Robitaille Y. Pelizaeus-Merzbacher disease. J Neuropathol Exp Neurol. 2002;61:747-59. doi: 10.1093/ jnen/61.9.747.
Torii T, Miyamoto Y, Yamauchi J, Tanoue A. Pelizaeus-Merzbacher disease: cellular pathogenesis and pharmacologic therapy. Pediatr Int. 2014;56:659-66. doi: 10.1111/ ped.12450.
Singh R, Samanta D. Pelizaeus-Merzbacher Disease. [Updated 2022 Feb 4]. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing; 2022.
Yeowell HN, Steinmann B. PLOD1-Related Kyphoscoliotic Ehlers-Danlos Syndrome. 2000 Feb 2 [Updated 2018 Oct 18]. In: Adam MP, Ardinger HH, Pagon RA, et al, editors. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2022.
Schiffmann R, van der Knaap MS. Invited article: an MRI-based approach to the diagnosis of white matter disorders. Neurology. 2009;72:750-9. doi:10.1212/01. wnl.0000343049.00540.c8
Barkovich AJ, Deon S. Hypomyelinating disorders: An MRI approach. Neurobiol Dis. 2016;87:50-58. doi:10.1016/j. nbd.2015.10.015