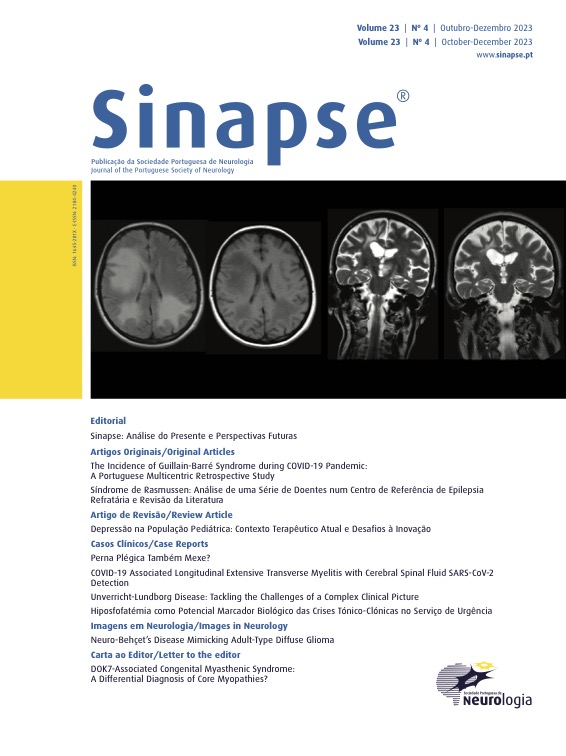
Rasmussen’s Syndrome: Case-Series Study from a Refractory Epilepsy Reference Center and Revision of Literature
DOI:
https://doi.org/10.46531/sinapse/AO/230070/2023Keywords:
Child, Encephalitis/diagnostic imaging, Encephalitis/drug therapy, Encephalitis/physiopathologyAbstract
Introduction: Rasmussen’s syndrome (RS) is a rare immunomediated disease of childhood-predominant onset, presenting with refractory epilepsy and neurological deficits associated to progressive brain hemiatrophy. Its pathophysiological mechanisms are not well understood, and the effect of immunotherapy is not ascertained. Hemispheric surgery is an efficacious therapy for epilepsy, despite focal and cognitive sequelae. Curative treatment and ideal timing for surgery are still not defined. Our study aim is to describe a pediatric case-series with RS evaluated in a Reference Center for Refractory Epilepsy and compare our results with the available literature.Methods: Review of clinical, neurophysiological, radiological, therapeutics and prognosis characteristics of pediatric patients evaluated in our center with RS since 2006.
Results: Eight children were included (median age of onset 8.0 years), seven with left hemisphere dysfunction. Up until surgery/present moment, four presented epilepsia partialis continua, six had focal deficits and four had cognitive decline. Most patients revealed unilateral atrophy and T2/FLAIR hyperintensity with frontal predominance in the last magnetic resonance imaging (MRI). In the last video-EEG, all patients had ipsilateral interictal epileptiform activity and one had contralateral epileptiform activity as well. PET/SPECT was used in three patients and functional MRI in one patient for language lateralization. Four were submitted to surgery (three hemispherectomies, one frontal resection), having all previously done immunoglobulin, three corticosteroids and two tacrolimus. In the first year post-surgery, two patients were seizure-free, with the others with a significant improvement of their seizures; the patient submitted to frontal resection did not present surgical sequelae, with the remaining having motor and cognitive sequelae (albeit one with language improvement). Among patients not submitted to surgery, all maintain refractory epilepsy with at least four antiseizure drugs, with immunoglobulin been used in three patients, corticosteroids in two and tacrolimus in one.
Conclusion: The management of RS is challenging regarding the balance between seizure control and the neurological surgical deficits. Our sample reflects the literature data, according to which hemispherectomy is the most effective therapy for seizure control, despite causing significant morbidity, rising questions about its timing.
Downloads
References
Rasmussen T, Olszewski J, Lloyd-Smith D. Focal seizures due to chronic localized encephalitis. Neurology. 1958;8:435-5. doi:10.1212/wnl.8.6.435
Cay-Martinez K, Hickman R, II GM, Provenzano F, Sands T. Rasmussen Encephalitis: An Update. Semin Neurol. 2020;40:201-10. doi:10.1055/s-0040-1708504
Varadkar S, Bien CG, Kruse CA, Jensen FE, Bauer J, Pardo CA, et al. Rasmussen’s encephalitis: clinical features, pathobiology, and treatment advances. Lancet Neurol. 2014;13:195-205. doi:10.1016/s1474-4422(13)70260-6
Bien CG, Granata T, Antozzi C, Cross JH, Dulac O, Kurthen M, et al. Pathogenesis, diagnosis and treatment of Rasmussen encephalitisA European consensus statement. Brain. 2005;128:454-71. doi:10.1093/brain/awh415
Bien CG, Widman G, Urbach H, Sassen R, Kuczaty S, Wiestler OD, et al. The natural history of Rasmussen’s encephalitis. Brain. 2002;125:1751-9. doi:10.1093/brain/awf176
Bien CG, Urbach H, Deckert M, Schramm J, Wiestler OD, Lassmann H, et al. Diagnosis and staging of Rasmussen’s encephalitis by serial MRI and histopathology. Neurology. 2002;58:250-7. doi:10.1212/wnl.58.2.250
Chiapparini L, Granata T, Farina L, Ciceri E, Erbetta A, Ragona F, et al. Diagnostic imaging in 13 cases of Rasmussen’s encephalitis: can early MRI suggest the diagnosis? Neuroradiology. 2003;45:171-83. doi:10.1007/s00234-002-0923-7
Longaretti F, Dunkley C, Varadkar S, Vargha‐Khadem F, Boyd SG, Cross JH. Evolution of the EEG in children with Rasmussen’s syndrome. Epilepsia. 2012;53:1539-45. doi:10.1111/j.1528-1167.2012.03565.x
Kuki I, Matsuda K, Kubota Y, Fukuyama T, Takahashi Y, Inoue Y, et al. Functional neuroimaging in Rasmussen syndrome. Epilepsy Res. 2018;140:120-7. doi:10.1016/j.eplepsyres.2018.01.001
Ganesan K, Ursekar M. Clinical utility of BOLD fMRI in preoperative work-up of epilepsy. Indian J Radiology Imaging. 2014;24:22-36. doi:10.4103/0971-3026.130688
Pardo CA, Vining EPG, Guo L, Skolasky RL, Carson BS, Freeman JM. The Pathology of Rasmussen Syndrome: Stages of Cortical Involvement and Neuropathological Studies in 45 Hemispherectomies. Epilepsia. 2004;45:516-26. doi:10.1111/j.0013-9580.2004.33103.x
Tang C, Luan G, Li T. Rasmussen’s encephalitis: mechanisms update and potential therapy target. Ther Adv Chronic Dis. 2020;11:2040622320971413. doi:10.1177/2040622320971413
Olson HE, Lechpammer M, Prabhu SP, Ciarlini PD, Poduri A, Gooty VD, et al. Clinical application and evaluation of the Bien diagnostic criteria for Rasmussen encephalitis. Epilepsia. 2013;54:1753-60. doi:10.1111/epi.12334
Riney K, Bogacz A, Somerville E, Hirsch E, Nabbout R, Scheffer IE, et al. International League Against Epilepsy classification and definition of epilepsy syndromes with onset at a variable age: position statement by the ILAE Task Force on Nosology and Definitions. Epilepsia. 2022;63:1443-74. doi:10.1111/epi.17240
Liba Z, Vaskova M, Zamecnik J, Kayserova J, Nohejlova H, Ebel M, et al. An immunotherapy effect analysis in Rasmussen encephalitis. BMC Neurol. 2020;20:359. doi:10.1186/s12883-020-01932-9
Engel JJ, Ness PV, Rasmussen T, Ojemann L. Outcome with respect to epileptic seizures. In: Engel J, editor. Surgical Treatment of the Epilepsies. New York: Raven Press; 1993. p.609–21.
Benjamin RN, Thomas M, Muthusamy K, Yoganathan S, Mathew V, Chacko AG, et al. Age-Dependent Reduction in Severity and Discrete Topographical Patterns in Rasmussen Encephalitis: A Link to Cortical Maturation? Pediatr Neurol. 2020;112:25-33. doi:10.1016/j.pediatrneurol.2020.07.016
Borne A, Perrone-Bertolotti M, Jambaqué I, Castaignède C, Dorfmüller G, Ferrand-Sorbets S, et al. Cognitive outcome after left functional hemispherectomy on dominant hemisphere in patients with Rasmussen encephalitis: beyond the myth of aphasia. Patient series. J Neurosurg Case Lessons. 2022;4:CASE22410. doi:10.3171/case22410
Bulteau C, Grosmaitre C, Save-Pédebos J, Leunen D, Delalande O, Dorfmüller G, et al. Language recovery after left hemispherotomy for Rasmussen encephalitis. Epilepsy Behav. 2015;53:51-7. doi:10.1016/j.yebeh.2015.07.044
Villarejo-Ortega F, García-Fernández M, Castillo CF, Fabregate-Fuente M, Álvarez-Linera J, De Prada-Vicente I, et al. Seizure and developmental outcomes after hemispherectomy in children and adolescents with intractable epilepsy. Child’s Nerv Syst. 2013;29:475-88. doi:10.1007/s00381012-1949-8
Basheer SN, Connolly MB, Lautzenhiser A, Sherman EM, Hendson G, Steinbok P. Hemispheric surgery in children with refractory epilepsy: seizure outcome, complications, and adaptive function. Epilepsia. 2007;48:133-40. doi:10.1111/j.1528-1167.2006.00909.x
Wagner J, Schoene‐Bake J, Bien CG, Urbach H, Elger CE, Weber B. Automated 3D MRI volumetry reveals regional atrophy differences in Rasmussen encephalitis. Epilepsia. 2012;53:613-21. doi:10.1111/j.1528-1167.2011.03396.x
Bingaman JR, Sundar SJ, Hsieh JK, Lu E, Jehi L, Wyllie E, et al. The Clinical Utility of Surgical Histopathology in Predicting Seizure Outcomes in Patients with Rasmussen Encephalitis Undergoing Hemispherectomy. World Neurosurg. 2022;162:e517-e525. doi:10.1016/j.wneu.2022.03.043
Granata T, Gobbi G, Spreafico R, Vigevano F, Capovilla G, Ragona F, et al. Rasmussen’s encephalitis: Early characteristics allow diagnosis. Neurology. 2003;60:422-5. doi:10.1212/wnl.60.3.422
So N, Gloor P. Electroencephalographic and electrocorticographic findings in chronic encephalitis of the Rasmussen’s type. In: Andermann F, Rasmussen T, editor. Chronic Encephalitis and Epilepsy: Rasmussen’s Syndrome. Boston: Buttherworth-Hainemann; 1991. p.37–45.
Bien CG, Tiemeier H, Sassen R, Kuczaty S, Urbach H, von Lehe M, et al. Rasmussen encephalitis: Incidence and course under randomized therapy with tacrolimus or intravenous immunoglobulins. Epilepsia. 2013;54:543-50. doi:10.1111/epi.12042
Bien CG, Gleissner U, Sassen R, Widman G, Urbach H, Elger CE. An open study of tacrolimus therapy in Rasmussen encephalitis. Neurology. 2004;62:2106-9. doi:10.1212/01. wnl.0000128044.94294.87
Lagarde S, Boucraut J, Bartolomei F. Medical treatment of Rasmussen’s Encephalitis: A systematic review. Rev Neurol. 2022;178:675-91. doi:10.1016/j.neurol.2022.01.007
Takahashi Y, Yamazaki E, Mine J, Kubota Y, Imai K, Mogami Y, et al. Immunomodulatory therapy versus surgery for Rasmussen syndrome in early childhood. Brain Dev. 2013;35:778-85. doi:10.1016/j.braindev.2013.01.010
Liba Z, Muthaffar O, Tang J, Minassian B, Halliday W, Branson H, et al. Rasmussen encephalitis: response to early immunotherapy in a case of immune-mediated encephalitis. Neurology Neuroimmunol Neuroinflammation. 2015;2:e69. doi:10.1212/nxi.0000000000000069
Orsini A, Foiadelli T, Carli N, Costagliola G, Masini B, Bonuccelli A, et al. Rasmussen’s encephalitis: From immune pathogenesis towards targeted-therapy. Seizure. 2020;81:76-83. doi:10.1016/j.seizure.2020.07.023
Harris WB, Phillips HW, Chen JS, Weil AG, Ibrahim GM, Fallah A. Seizure outcomes in children with Rasmussen’s encephalitis undergoing resective or hemispheric epilepsy surgery: an individual participant data meta-analysis. J Neurosurg Pediatrics. 2020;25:274-83. doi:10.3171/2019.9.peds19380
Schramm J, Kuczaty S, Sassen R, Elger CE, Lehe M von. Pediatric functional hemispherectomy: outcome in 92 patients. Acta Neurochir. 2012;154:2017-28. doi:10.1007/s00701-012-1481-3
Santos MV, Teixeira TL, Ioriatti ES, Thome U, Hamad AP de A, Machado HR. Risk factors and results of hemispherotomy reoperations in children. Neurosurg Focus. 2020;48:E5. doi:10.3171/2020.1.focus19944
Sundar SJ, Lu E, Schmidt ES, Kondylis ED, Vegh D, Poturalski MJ, et al. Seizure Outcomes and Reoperation in Surgical Rasmussen Encephalitis Patients. Neurosurgery. 2022;91:93-102. doi:10.1227/neu.0000000000001958
Villani F, Didato G, Deleo F, Tringali G, Garbelli R, Granata T, et al. Long‐term outcome after limited cortical resections in two cases of adult‐onset Rasmussen encephalitis. Epilepsia. 2014;55:e38-e43. doi:10.1111/epi.12596
Alotaibi F, Albaradie R, Almubarak S, Baeesa S, Steven DA, Girvin JP. Hemispherotomy for Epilepsy: The Procedure Evolution and Outcome. Can J Neurological Sci. 2021;48:451-63. doi:10.1017/cjn.2020.216
Loddenkemper T, Wyllie E, Lardizabal D, Stanford LD, Bingaman W. Late Language Transfer in Patients with Rasmussen Encephalitis. Epilepsia. 2003;44:870-1. doi:10.1046/j.1528-1157.2003.66402.x
Telfeian AE, Berqvist C, Danielak C, Simon SL, Duhaime AC. Recovery of Language after Left Hemispherectomy in a Sixteen-Year-Old Girl with Late-Onset Seizures. Pediatr Neurosurg. 2002;37:19-21. doi:10.1159/000065096
Qun W, Zhanpeng Z, Guangming W, Jiqing Q, Lichao S. Functional hemispherectomy for adult rasmussen encephalitis: a case report and literature review. Turk Neurosurg. 2017;29(6):945-949. doi:10.5137/1019-5149.jtn.21188-17.1
Takei H, Wilfong A, Malphrus A, Yoshor D, Hunter JV, Armstrong DL, et al. Dual pathology in Rasmussen’s encephalitis: A study of seven cases and review of the literature. Neuropathology. 2010;30:381-91. doi:10.1111/j.1440-1789.2009.01079.x
Hart YM, Andermann F, Robitaille Y, Laxer KD, Rasmussen T, Davis R. Double pathology in Rasmussen’s syndrome. Neurology. 1998;50:731-5. doi:10.1212/wnl.50.3.731
Hohenbichler K, Lelotte J, Lhommel R, Tahry RE, Vrielynck P, Santos SF. Adult‐onset Rasmussen encephalitis associated with focal cortical dysplasia. Epileptic Disord. 2017;19:476-80. doi:10.1684/epd.2017.0947
Gilani A, Kleinschmidt-DeMasters BK. How frequent is double pathology in Rasmussen encephalitis? Clin Neuropathol. 2020;39:55-63. doi:10.5414/np301231
Gambardella A, Andermann F, Shorvon S, Piane EL, Aguglia U. Limited chronic focal encephalitis. Neurology. 2008;70:374-7. doi:10.1212/01.wnl.0000298723.96653.99
Rizek P, Cheung C, McLachlan RS, Hayman-Abello B, Lee DH, Hammond RR, et al. Childhood-onset nonprogressive chronic encephalitis. Epilepsy Behav. 2014;31:85-90. doi:10.1016/j.yebeh.2013.11.005
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Sinapse

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.