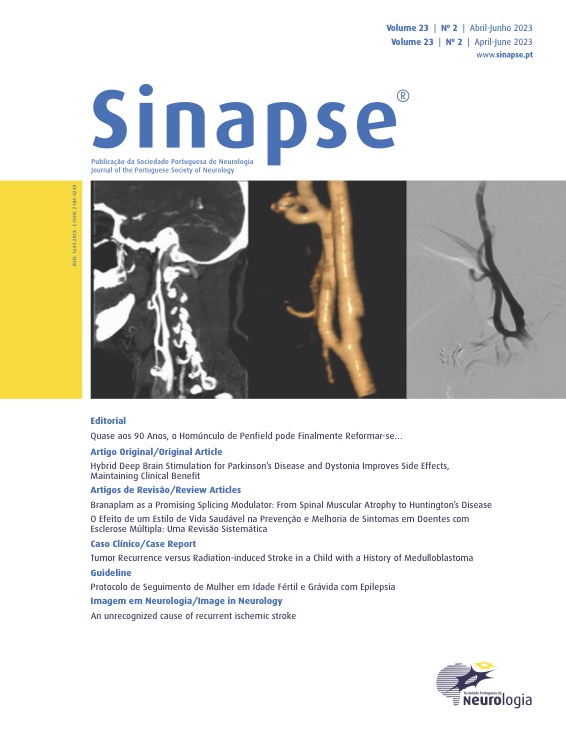
Tumor Recurrence versus Radiation-induced Stroke in a Child with a History of Medulloblastoma
DOI:
https://doi.org/10.46531/sinapse/CC/220076/2023Keywords:
Child, Medulloblastoma/radiotherapy, Radiation Injuries/ complications, Stroke/etiologyAbstract
Children with a history of central nervous system neoplasia, submitted to radiotherapy, have an increased risk of vascular complications that can be, clinically and imagiologically, very similar to a tumor recurrence. We describe the case of an 11-year-old child who, 10 years after diagnosis and treatment of a medulloblastoma, suddenly developed right hemiparesis. The initial imaging findings did not allow the exclusion of tumor recurrence, making a differential diagnosis with recent ischemic injury. Due to clinical and imaging worsening, the patient started chemotherapy, suspended after the first cycle, due to clear neurological improvement. One month after the onset of symptoms, patient was clinically stable, having undergone a new magnetic resonance imaging, revealing a chronic evolution of the lesion, suggestive of a vascular etiology. This case explores the differential diagnosis of late tumor recurrence in children undergoing radiotherapy, highlighting the importance of etiological identification in therapeutic guidance.Downloads
References
Mueller S, Fullerton HJ, Stratton K, Leisenring W, Weathers RE, Stovall M, et al. Radiation, atherosclerotic risk factors, and stroke risk in survivors of pediatric cancer: a report from the Childhood Cancer Survivor Study. Int J Radiat Oncol Biol Phys. 2013;86:649-55. doi: 10.1016/j.ijrobp.2013.03.034.
Murphy ES, Xie H, Merchant TE, Yu JS, Chao ST, Suh JH. Review of cranial radiotherapy-induced vasculopathy. J Neurooncol. 2015;122:421-9. doi: 10.1007/s11060-015-1732-2.
Kim JH, Brown SL, Jenrow KA, Ryu S. Mechanisms of radiation-induced brain toxicity and implications for future clinical trials. J Neurooncol. 2008;87:279-86. doi: 10.1007/ s11060-008-9520-x.
Twitchell S, Karsy M, Guan J, Couldwell WT, Taussky P. Sequelae and management of radiation vasculopathy in neurosurgical patients. J Neurosurg. 2018:1-9. doi: 10.3171/2017.12.JNS172635.
Omuro AM, Leite CC, Mokhtari K, Delattre JY. Pitfalls in the diagnosis of brain tumours. Lancet Neurol. 2006;5:937-48. doi: 10.1016/S1474-4422(06)70597-X.
Verma N, Cowperthwaite MC, Burnett MG, Markey MK. Differentiating tumor recurrence from treatment necrosis: a review of neuro-oncologic imaging strategies. Neuro Oncol. 2013;15:515-34. doi: 10.1093/neuonc/nos307.
Omura M, Aida N, Sekido K, Kakehi M, Matsubara S. Large intracranial vessel occlusive vasculopathy after radiation therapy in children: clinical features and usefulness of magnetic resonance imaging. Int J Radiat Oncol Biol Phys. 1997;38:241-9. doi: 10.1016/s0360-3016(97)82497-2.
Tanyildizi Y, Keweloh S, Neu MA, Russo A, Wingerter A, Weyer-Elberich V, et al. Radiation-induced vascular changes in the intracranial irradiation field in medulloblastoma survivors: An MRI study. Radiother Oncol. 2019;136:50-5. doi: 10.1016/j.radonc.2019.03.017.
Haddy N, Mousannif A, Tukenova M, Guibout C, Grill J, Dhermain F, et al. Relationship between the brain radiation dose for the treatment of childhood cancer and the risk of long-term cerebrovascular mortality. Brain. 2011;134:1362-72. doi: 10.1093/brain/awr071.
Finelli PF. Diagnostic approach to restricted-diffusion patterns on MR imaging. Neurol Clin Pract. 2012;2:287-93. doi: 10.1212/CPJ.0b013e318278bee1.
Bansal LR, Belair J, Cummings D, Zuccoli G. Late-onset radiation-induced vasculopathy and stroke in a child with medulloblastoma. J Child Neurol. 2015;30:800-2. doi: 10.1177/0883073814538501.
Grenier Y, Tomita T, Marymont MH, Byrd S, Burrowes DM. Late postirradiation occlusive vasculopathy in childhood medulloblastoma – report of two cases. J Neurosurg. 1998;89:460-4. doi: 10.3171/jns.1998.89.3.0460.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.